Research
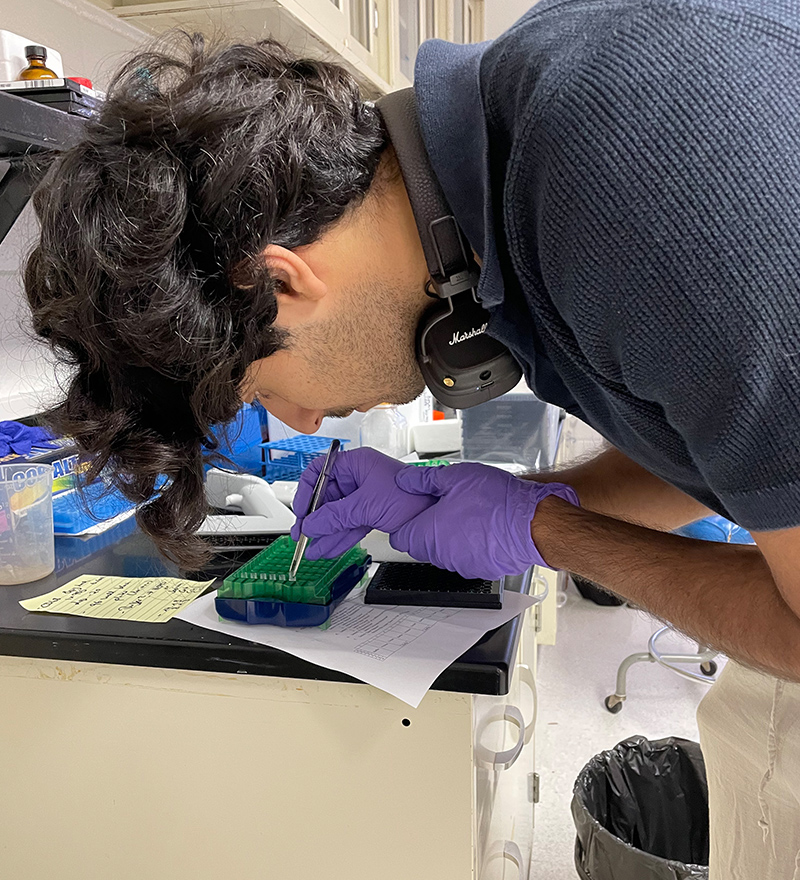
Research in the Marquez-Nostra lab focuses on the development of radiolabeled antibodies for positron emission tomography (PET) and single-photon emission computed tomography (SPECT) imaging of cancer in animal models with the goal of translating our radiopharmaceuticals to clinical studies.
This approach has the potential to predict response to corresponding targeted therapy in a noninvasive way, to understand what makes different cancers resistant to targeted therapies, and to develop new treatments to overcome resistance. We are a highly collaborative team and we partner with industry, clinicians, and other basic scientists to accomplish our goals. Trainees in the lab learn a variety of skills that interface radiochemistry, chemistry, cancer biology, biochemistry, and immunobiology.
CURRENT PROJECTS
Imaging the
multifaceted response
to a bispecific antibody therapy.
Resistance to standard of care treatments contributes to mortality in patients with metastatic non-small cell lung cancer (NSCLC). Metastatic NSCLC often harbors mutations in the epidermal growth factor receptor (EGFR), in which patients frequently develop resistance to EGFR tyrosine kinase inhibitors (TKI). MET gene amplification is a resistance mechanism for EGFR TKIs. To overcome resistance to EGFR TKI, a bispecific antibody called amivantamab was developed by Janssen Pharmaceuticals. Amivantamab was FDA-approved in 2021 for the treatment of metastatic NSCLC with EGFR exon 20 mutations.
Amivantamab targets both EGFR and cMET receptors concurrently, facilitating multiple mechanisms to inhibit tumor growth. Co-binding to these receptors inhibits receptor-ligand activation, and degrades these receptors upon antibody internalization, and recruits immune cells to kill cancer cells through trogocytosis and antibody mediated cellular toxicity. Currently, there are no effective methods to predict and monitor response to bispecific antibodies, making it difficult to select patients most likely to respond to this new therapy and save those unlikely to respond from unnecessary treatment.
Our goals are to develop PET imaging biomarkers to quantify the multifaceted response to amivantamab therapy in vivo. This project is funded by the National Cancer Institute (R01CA255226).
Development of
novel human Fab probes
for PET imaging of macrophages.
Macrophages are a class of immune cells important in the prognosis and treatment of several diseases, including cancer. CD68 is the established clinical biomarker for pan-macrophage. Currently, there are no non-invasive probes specific for human or mouse CD68. Structural differences between human and mouse orthologs of CD68 reduce the feasibility of developing one probe that is cross-reactive to both species with equivalent affinity and specificity. Developing a pair of probes with similar structure but with high affinity and specificity for each human and mouse CD68 targets can address these limitations. Further, discovery of novel probes using a fully human synthetic phage display Fab library is an established approach to discover and develop human Fabs with high target affinity and specificity, suitable for PET imaging. TIts companion PET probe for mouse CD68 can be used in preclinical studies to monitor macrophage trafficking because of new therapies to demonstrate proof-of-mechanism studies to justify clinical translation. Our short-term goal is to develop a pair of PET probes specific to mouse and to human CD68 for PET imaging of macrophages in vivo. This project is funded by the National Institute of Biomedical Imaging and Bioengineering (R01EB031821).
Dual-isotope SPECT imaging
and immunophenotyping
of T cells and macrophages
to determine response
to immunotherapy.
While significant progress has been made in the past decade with immunotherapy for metastatic melanoma and renal cell carcinoma (RCC), not all patients respond, and others develop resistance over time. Hundreds of novel regimens are being developed to overcome primary and acquired resistance. Some combinations increase the infiltration of cytotoxic T cells to tumor cells, while others modulate tumor-associated macrophages (TAMs) to their cancer-fighting function. However, toxicity to patients is an important limitation to immunotherapy regimens. Non-invasive imaging techniques are needed to determine response to combination therapy to save potential non-responders from unnecessary toxicity. Current imaging techniques do not assess the dynamic changes in the levels of T cells and TAMs at the same time. The goal of this project is to develop SPECT imaging agents for concurrent imaging of T cells and TAMs to understand the interplay between these immune cells in the context of combination therapy. This work is funded by the National Cancer Institute R01CA269349.